
Central serous chorioretinopathy (CSCR or CSR) is a disease that affects the retina and the retinal pigment epithelium (RPE). It is characterized by the collection of fluid under the central portion of the retina known as the macula. This small accumulation of fluid, similar to a blister, causes blurry vision. The fluid pools under the retina as a result of faulty RPE cells, which usually pump fluid away from the retina. Central serous chorioretinopathy affects 9.9 males and 1.7 females per 100,000 population (age adjusted) per year, and presents in two different varieties.
Two Varieties of CSR
The first tends to appear suddenly in one eye of younger (20-40 year old) males and most commonly (80-90%) resolves without treatment over 4-6 weeks. Patients often experience a smudge in the vision and objects may look smaller. This condition has a recurrence rate of approximately 40-50%.
The second occurs after the age of 50, with less preponderance to the male gender, affects both eyes, and does not easily resolve. There are often multiple areas of leaking not confined to the central retina and is sometimes referred to as multifocal CSR.
Contributing Factors
There are a few factors that may trigger CSR, the most common of which are:
- Stress
- Type A personality
- The administration of corticosteroids
- Increased systemic cortisol and epinephrine levels
Steroids and Central Serous Chorioretinopathy
There is a strong relationship between steroid medications and CSR and we always advise patients diagnosed with CSR to avoid unnecessary use of steroids.
If steroids are required, patients should be evaluated before and during any systemic use. Central serous chorioretinopathy has been reported even after injection of steroids into an inflamed joint.
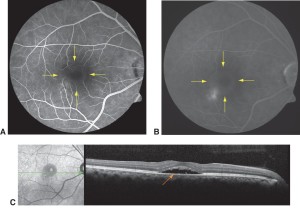
C: OCT image through the sub-retinal fluid, which appears as a dark void between the retina and RPE
Treatment Options
Since many patients heal spontaneously, observation is always the first option. If, after a period of conservative observation, there is no improvement or possible worsening, we then consider treatment with LASER.
Treatment has evolved from the use of a thermal (destructive) LASER to a less destructive or “cold” LASER using a technology known as photodynamic therapy (PDT).
Photodynamic therapy incorporates a special dye (Visudyne) that is injected in your arm and accumulates in abnormal tissue. The dye is then activated by the cold” LASER. Activated dye causes to a chemical reaction that closes the abnormal blood vessels instigating the retinopathy. There is no pain involved.
Before undergoing PDT patients undergo a thorough examination followed by diagnostic testing to rule out other possible diseases. As in any procedure there are risks involved with PDT that your physician will discuss with you before initiation of therapy.
In our experience PDT has a 90 % success rate even in the face of unfavorable factors like longstanding sub-retinal fluid or RPE detachment.
Other treatment options are currently being evaluated and include: pulsed diode laser, intravitreal anti-VEGF injection, and oral medications.
What to do?
If you have any questions about your retinal condition, contact your retina specialist or schedule an appointment with one of our doctors for a thorough consultation.
